GP information
Please follow this link for the up to date GP information: https://bomss.org/gp-hub/
10 Top Tips For GP
Management Of Patients
Post Bariatric Surgery
10 Top Tips to Help GP and Primary Care Staff
Tip 1: Keep a register of bariatric surgery patients. It is important to record the type of procedure in the register as the different procedures have
different risk of nutritional deficiencies.
Tip 2: Encourage patients to check their own weight and diet and to attend annual BMI and diet reviews with a health care professional
Tip 3: Symptoms of continuous vomiting, dysphagia, intestinal obstruction (gastric bypass) or severe abdominal pain requires emergency
admission under the surgical team.
Tip 4: Continue to review comorbidities post surgery, including diabetes, hypertension, hypercholesterolemia and obstructive sleep apnoea, as well
as mental health
Mental health
There is a higher rate of mental health problems in people with severe and complex obesity compared to general population. The psychological
management of these people can be complex there should be a low threshold for referral to specialist mental health teams.
Tip 5: Review the patient’s regular medication
- The formulations may need adjustment post-surgery to allow for changes in bioavailability.
- Review comorbidity medications, such as antihypertensive, diabetes medication etc post surgery.
- Requirements are likely to fall with postoperative weight loss but may increase later if weight loss is not maintained.
- Consider pill size – patients may need liquid formulations or syrups in the immediate postoperative period. However usual medication formulations should be tolerated by around 6 weeks postoperatively.
- Replace extended-release formulations with immediate- release formulations
- Psychiatric medications may need increased or divided doses
- Use diuretic with caution due to the increased risk of hypokalaemia
- Monitor anticoagulants carefully
- Avoid non steroidal anti- inflammatory drugs if no alternative use only with a proton pump inhibitor.
- Avoid bisphosphonates
- Patients with gastric bands should avoid effervescent medication
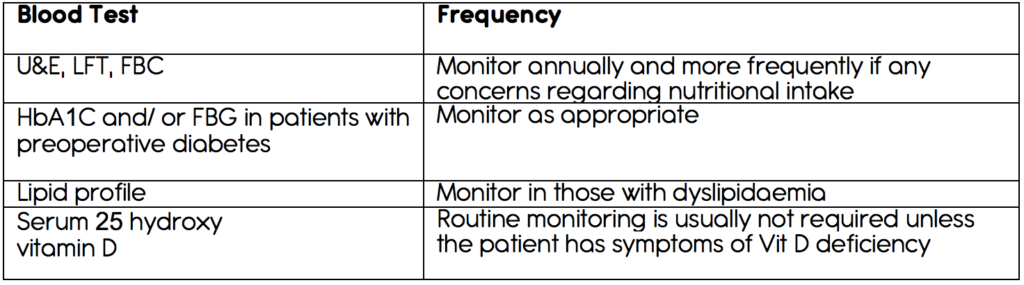
Tip 6: Bariatric surgery patients require lifelong annual blood test, including micronutrient monitoring. Encourage patients to attend their annual
blood tests.
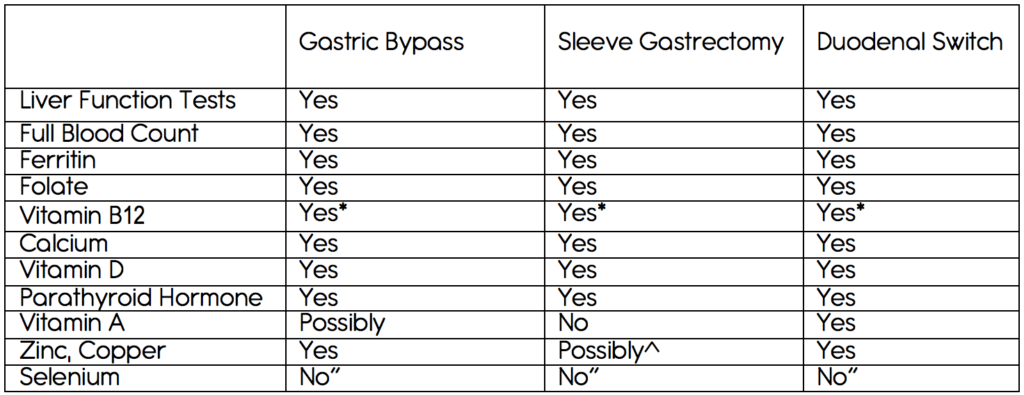
*if the patient is having 3-monthly intramuscular injections of vitamin b12, there may be no need for annual checks.
^if the patient has had a long-limb bypass or has symptoms of steatorrhoea or night blindness.
“Measure when there are deficiency concerns (see top tip seven).
Tip 7: Be aware of potential nutritional deficiencies that may occur and their signs and symptoms.
In particular, patients are at risk of anaemia and vitamin d deficiency as well as protein malnutrition and other vitamin and micronutrient
deficiencies; if a patient is deficient in one nutrient, they are likely to be deficient in others as well.
Tip 8: Ensure the patient is taking the appropriate lifelong nutritional supplements as recommended by the bariatric centre.
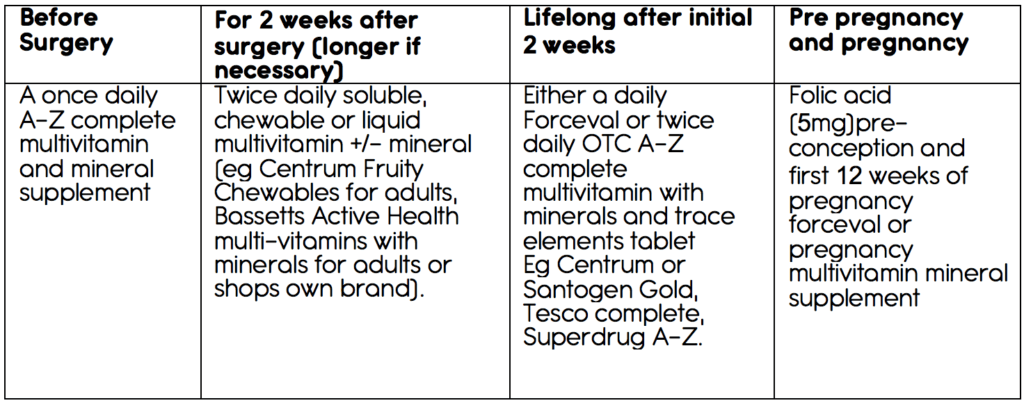
Tip 9: Discuss contraception – ideally, pregnancy should be avoided for at least 18-24 months post surgery.
A long acting reversible contraceptive of the patient’s choice would be appropriate. Oral contraception and the depo-provera are not
recommended because if the issue with absorption and weight gain, respectively.
Tip 10: If a patient, should plan or wish to become pregnant after bariatric surgery, alter their nutritional supplements to one suitable during
pregnancy. Pregnacare or a supplement for pregnancy support
Gastric bands may need band adjustments on becoming pregnant to allow good nutritional intake and fetal growth and symptom control .
